Articles
Exposure to pollution causes 10% of all cancer cases in Europe - EEA (European Evironment Agency)
Exposure to air pollution, second-hand smoke, radon, ultraviolet radiation, asbestos, certain chemicals and other pollutants causes over 10% of all cancer cases in Europe, according to a European Environment Agency (EEA) report published today. The good news is that these risks are preventable.
“Pollutants in the environment and at the workplace, as well as some natural risks, have a huge impact on our health, and in some cases lead to cancer, according to the EEA web report 'Beating cancer — the role of Europe’s environment'. With nearly 3 million new patients and 1.3 million deaths each year across the European Union, cancer takes a huge toll on our society. The economic costs are also enormous, estimated at around EUR 178 billion in 2018 alone.”
“For the first time, the EEA investigated the links between cancer and the environment, reviewing the latest scientific evidence on air pollution, radon, ultraviolet radiation, second-hand smoke and chemicals. The report estimates that environmental and occupational risks lie behind around 10% of cancer cases in Europe.”
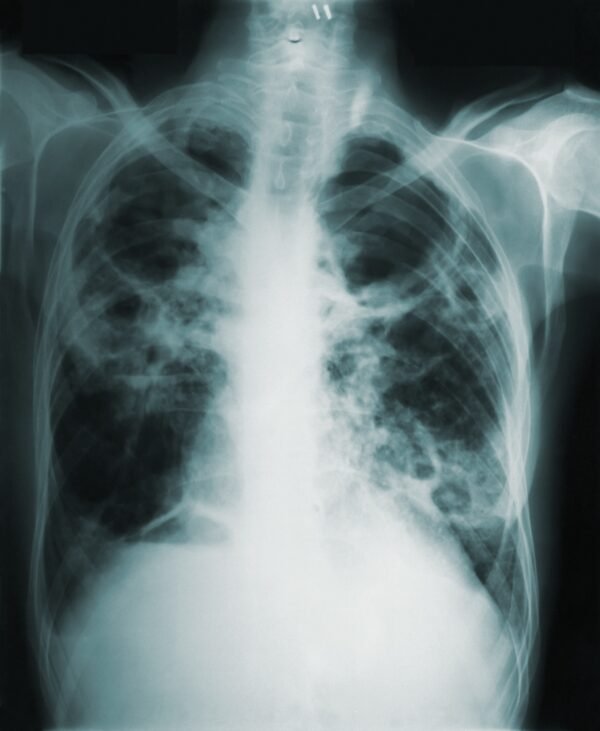
“Air pollution (both indoor and outdoor) is linked to around 1% of all cancer cases in Europe, and causes around 2% of all cancer deaths. For lung cancers alone, this rises to 9% of deaths. Recent studies have detected associations between long term exposure to particulate matter, a key air pollutant, and leukaemia in adults and children.”
“Exposure to second-hand smoke may increase the overall risk for all cancers by up to 16% in people who have themselves never been smokers. Around 31% of Europeans are exposed to second-hand tobacco smoke at home, at work, during leisure, in educational institutions or in public settings.”
“Certain chemicals used in European workplaces and released into the environment are carcinogenic and contribute to causing cancer. Moreover, several of these chemicals are known or suspected to induce cancer in multiple organs, including lead, arsenic, chromium, cadmium, acrylamide, pesticides, Bisphenol A and per- and polyfluorinated alkyl substances (PFAS).”
All forms of asbestos are well-known carcinogens, associated with mesothelioma and lung cancers, as well as laryngeal and ovarian cancers. While the EU banned asbestos in 2005, it remains present in buildings and infrastructure leading to the exposure of workers involved in renovation and demolition work. In addition, cancers continue to manifest many years after exposure, with asbestos estimated to account for 55-88% of occupational lung cancers.”
The First Four Healthy Building Strategies - The Lancet COVID-19 Commission
Full Article Title:
The First Four Health Building Strategies Every Building Should Pursue to Reduce Risk from COVID-19
July 2022 - The Lancet COVID-19 Commission Task Force on Safe Work, Safe School, and Safe Travel
“Understanding of the most probable transmission routes and identifying the risk environment for disease spread should always be among the first critical steps in the response to future disease threats.”…
“Laboratory, field, modeling, and case studies have demonstrated that airborne transmission via inhalation of virus-laden aerosols is important, if not dominant, for COVID-19”…
“To combat the risk of airborne transmission of COVID-19, control strategies that reduce the concentration of (and therefore, the likelihood of inhaling) potentially infectious respiratory aerosols must be implemented. Increased outdoor air ventilation to dilute aerosols and reduce their concentration and/or enhanced filtration efficiency to remove particles from recirculated air have been shown to be effective as part of an overall strategy to reduce risk. These strategies should be prioritized in occupied environments in which aerosols accumulate most rapidly: indoor spaces with low outdoor air ventilation and/or low levels of (or no) filtration.”…
Effectively Managing the Risk of Airborne Pathogens in Healthcare - Knowlex Webinar
Webinar Description:
After the significant interest in their opening keynote at the recent IPC Conference in Birmingham, the have partnered with title sponsor PRS Ltd (Pathogen Reduction Systems) to invite you to an exclusive webinar to explore in more detail, the effective management of airborne pathogens in healthcare.
This highly informative webinar speaks on air filtration, ventilation, and the necessities of air purifiers featuring HEPA filters and Ultra-Violet Type-C Light.
SPOTTED: YouTuber Colin Furze with his custom MedicAir Air Purifier
Colin Furze has nearly 12 million YouTube subscribers. His YouTube channel is full of crazy inventions and so much more.
Popular YouTuber Colin Furze with his custom MedicAir air purifier in the background of his most recent video.
We Need to Improve Indoor Air Quality: Here’s How and Why - Scientific American
Upgrading buildings’ ventilation, filtration and other factors would not only decrease COVID transmission but also improve health and cognitive performance in general
Air purification device stands in a classroom at an elementary school in Berlin. Credit: Annette Riedl/dpa/Alamy Live News
We spend 90 percent of our lives indoors, yet most of us seldom spare a thought for the quality of the air we breathe there.
More than a century ago, pioneering nurse and statistician Florence Nightingale proclaimed the importance of open air and bedroom ventilation for tuberculosis patients. Today in Nordic countries, it is common practice to let babies nap outside, sometimes in freezing temperatures. But even though humans have long attributed health benefits to fresh outdoor air, it is a lesson many of us seemed to have largely forgotten—until the COVID-19 pandemic forced us to relearn it.
It is now widely acknowledged that SARS-CoV-2, the virus that causes COVID, is frequently transmitted by airborne droplets called aerosols that hang in the air and can travel over short and long distances. “This is a virus that spreads through the air almost exclusively indoors. If we start there, then the building matters,” says Joseph Allen, an associate professor at the Harvard T. H. Chan School of Public Health and director of its Healthy Buildings program.
As the U.S. and many other countries drop mask mandates and other short-term measures to help reduce the spread of SARS-CoV-2, improving indoor air quality is becoming even more crucial. “As we start to shift away from these broad government mandates and regulations, we need strategies ... that are passive, that are operating in the background,” Allen says. “Clean air shouldn’t be partisan.”
Cleaner indoor air has other benefits besides reducing COVID risk. Influenza and other respiratory viruses also spread through the air and cause a huge amount of illness and lost productivity. Plus, studies have shown that poor ventilation has all kinds of other health effects, from “sick building syndrome” to cognitive impacts.
Perhaps society could take a lesson from the way it regards water treatment. Extensive measures are taken to ensure water quality in public systems. Why not do the same for air?
For the most part, “we don’t rely on people in the U.S. to filter their water individually; we provide clean, safe drinking water,” says Linsey Marr, a professor of civil and environmental engineering at Virginia Tech and a leading expert on aerosol transmission of viruses. “I think it’s time to start thinking about our indoor air in the same way.”
““ACCEPTABLE” AIR QUALITY”
In the past 40 years or so, engineers have designed buildings to have tighter “envelopes”—meaning they allow less air exchange with the outside—in order to improve energy efficiency, according to Allen. But the upshot of this is that many of our buildings are now optimized germ factories.
Much attention is paid to the quality of outdoor air—that is one of the main roles of the U.S. Environmental Protection Agency. But people spend much more time indoors, where we are routinely exposed not just to environmental pollutants but to indoor ones ranging from pathogens to cooking fumes to chemicals released by furniture.
“Humans are incredible indoor creatures,” says Richard Corsi, dean of the College of Engineering at the University of California, Davis. The average U.S. lifespan before the pandemic was about 79 years, and “we spend 69 years inside buildings.” Of that, Corsi notes, “54 years are spent inside of homes.”
The American Society of Heating and Air-Conditioning Engineers (ASHRAE) is a U.S. industry body that sets standards for what it calls “acceptable indoor air quality.” For nonresidential buildings, this is defined as “air in which there are no known contaminants at harmful concentrations, as determined by cognizant authorities, and with which a substantial majority (80 percent or more) of the people exposed do not express dissatisfaction.” For residential buildings, the definition is “air toward which a substantial majority of occupants express no dissatisfaction with respect to odor and sensory irritation and in which there are not likely to be contaminants at concentrations that are known to pose a health risk.”
Allen says building designers and managers should be striving for something better than merely “acceptable.” These standards are “well below” what is needed to protect against COVID, influenza and other infectious diseases, he says. Others agree. “Think about if somebody’s selling a car and used that kind of advertising: ‘Purchase our car; it will be acceptable to you,’” Corsi says. “I don’t think a lot of people would buy that car.”
ASHRAE standards aim to limit exposure to harmful substances with known exposure limits, such as formaldehyde and other volatile organic compounds, but not to pathogens—for which there are far fewer data—according to William P. Bahnfleth, chair of the ASHRAE Epidemic Task Force and a professor of architectural engineering at Pennsylvania State University. “Current minimum ventilation rates—alone—do not provide complete mitigation of airborne disease transmission risk,” Bahnfleth wrote in an e-mail to Scientific American. He added that although transmission risk cannot be reduced to zero, combining precautions such as vaccination, mask use and occupancy limits with engineering practices, including ventilation, filtration and air disinfection, “is the most effective way to minimize risk.”
Changing air quality standards takes time. Meanwhile some steps can be taken immediately to improve the air we breathe indoors. These steps involve strengthening four main pillars of indoor air quality: source control, ventilation, filtration and disinfection.
SOURCE CONTROL
In 1858 chemist Max von Pettenkofer, one of the pioneers of the indoor air quality movement, wrote that if a space contains a pile of manure, one should not try to remove the odor by ventilation but rather remove the manure.
In modern, broader terms, this means that people can prevent pollutants from being released into the air in the first place by limiting potential sources. For example, one could reduce cooking fumes by using an electric stove instead of a gas one.
When it comes to pathogens like SARS-CoV-2, a person who has been knowingly exposed could wear a high-quality mask or could stay home if they have any symptoms.
Of course, such measures alone cannot prevent all pathogens or other pollutants from entering the air, which is why other steps are needed.
VENTILATION
A building’s ventilation level refers to how much fresh outdoor air is being brought in; this fresh air dilutes the concentration of virus-laden particles in the air. Imagine a SARS-CoV-2 particle indoors as a drop of food coloring in a cup of water. Outdoors, it is more like a drop of dye in the ocean—it rapidly becomes so diluted as to be undetectable. Ventilation makes the indoor “cup” more like the outdoor “ocean.”
The simplest and cheapest way to improve ventilation is to open a window, but that is not always a viable option—especially if the air outside is more polluted than that inside. “This is a huge equity issue. Not everyone can open the windows and bring in fresh air,” says Kimberly Prather, an atmospheric chemist and professor at the Scripps Institution of Oceanography and the University of California, San Diego. People of color, for example, are more likely to live and work in places where they are exposed to harmful pollution. Wildfire smoke also frequently creates poor air quality in many parts of the western U.S.
Aside from windows, another source of indoor airflow is a heating, ventilation and air conditioning (HVAC) system. Most of these systems allow a building manager to vary the amount of fresh air intake. It should generally be set to maximum, experts say—provided the outdoor air quality is safe. Yet many buildings, especially before the pandemic, have had their HVAC system set to recirculate old, stale air. A good rule of thumb is to aim for having at least six air exchanges per hour through ventilation or the equivalent amount of fresh air through filtration.
One way to assess the amount of ventilation in a space is to use a carbon dioxide monitor. Humans exhale CO2 when we breathe, so levels of this gas provide a good proxy for how diluted the air is. Values below about 800 parts per million are potentially well ventilated, according to the U.S. Centers for Disease Control and Prevention.
CO2 meters such as this one in a restaurant in Galicia, Spain, can serve as a proxy for the amount of ventilation in a building. Numbers below 800 parts per million indicate a good amount of air exchange. Credit: M. Dylan/Europa Press via Getty Images
FILTRATION
Filtration involves removing particles and other pollutants from the air. A standard called minimum efficiency reporting values (MERV) offers a way of comparing different filters. The gold standard filter is a high-efficiency particulate air (HEPA) filter, which can remove 99.97 percent of airborne particles that are 0.3 micron in size, and an even greater percentage of larger or smaller particles (both of which are trapped more efficiently). HEPA is equivalent to a rating of MERV 17 or higher. Prather and Corsi both recommend upgrading filters to at least MERV 13 for most indoor settings such as schools or offices. Many HVAC systems can be upgraded to this standard—but some very old ones may have trouble with higher-efficiency filters, and this could cause air to leak around the filters, so it’s a good idea to check with an HVAC expert.
If the building in question does not have an HVAC system—many homes, for example, do not—one option is to purchase one or more portable air cleaners. These devices generally work well, provided they are the appropriate size for a room. They can be run at high speed to filter the air more quickly during specific times such as a party or when someone in the family is sick with COVID.
Portable air cleaners are not cheap, however; a good quality model starts at around $200, and the price goes up from there. Fortunately, some researchers have come up with a more affordable solution known as a Corsi-Rosenthal box. Named after U.C. Davis’s Corsi and Jim Rosenthal, CEO of filter manufacturer Tex-Air Filters, who both helped develop the idea, it is basically a DIY air cleaner made up of a box fan and four or five MERV filters duct-taped together. Instructions for building these boxes are available online, and they work surprisingly well. A Corsi-Rosenthal box in a 200-square-foot (about 19-square-meter) dorm room achieved the equivalent of about 24 air exchanges per hour—on par with a typical U.S. hospital and better than most similarly sized portable air cleaners. This is because, even though a Corsi-Rosenthal box’s filtration efficiency is lower than that of the HEPA filters in most portable air cleaners, the flow rate is much greater, thanks to the large fan. The only complaint is the noise, but Corsi and his colleagues are working on quieter designs.
AIR DISINFECTION
Finally, there is air disinfection: inactivating viruses using ultraviolet light. This is best for high-risk environments such as hospitals or school cafeterias, Virginia Tech’s Marr says. It works by shining UV light across the top of a room, which neutralizes airborne pathogens as they circulate through that space. Some wavelengths of UV light are harmful to humans, although there is a wavelength called far UVC that may be safer for people.
Most UV systems are expensive to install, however. And there’s a lot of snake oil out there. “If it sounds too good to be true,” Marr says, “it probably is.” For most homes and small businesses, focusing on ventilation and filtration is probably the easiest way to improve air quality.
INVESTING IN BETTER AIR
The Biden administration recently called on building managers in schools, universities and other settings to improve air indoor quality and also held a public briefing to draw attention to the importance of clean indoor air. Upgrading air quality can be expensive, but there are federal funds to support such efforts. According to a White House statement, the American Rescue Plan contains $122 billion to help schools stay open and $350 billion for state, local and tribal governments to upgrade ventilation and other infrastructure in local establishments and businesses.
“It’s a massive win to have the White House signal that healthy buildings are one of the pillars of pandemic response,” says Harvard’s Allen.
COVID has injected momentum into efforts to improve air quality inside buildings, and experts hope this momentum will result in lasting investments in this area.
“I think we are on the cusp of a new awareness about indoor air quality,” Marr says. “It’s so bad in many places that there’s lots of room for improvement.” Upgrading buildings will require an investment, Marr adds, but one that “I believe will pay off in terms of improved health and productivity.”
Article Title:
We Need to Improve Indoor Air Quality: Here's How and Why
Author:
Tanya Lewis
Publication:
Scientific American
Publisher:
SCIENTIFIC AMERICAN, a Division of Springer Nature America, Inc.
Date:
Jun 8, 2022
Copyright © 2022, Scientific American, Inc.
Ambient and indoor air pollution limits young people’s lung function - Air Quality News
Read the article directly here.
More evidence has emerged showing poor air quality directly leads to significant health problems, with worse effects among lower age groups.
A new study focused on South India, led by researchers at the Barcelona Institute for Global Health (ISGlobal), has identified a link between air pollution and poor lung function in young adults who had recently attained maximum lung function.
Published in Environment International, results point to worse lung performance with higher ambient and household air pollution. Although this sounds logical, up until recently studies of this kind have been limited, with scarce data on the health effects of ambient air pollution in lower-middle-income countries, specifically on young adults whose respiratory growth is peaking.
‘There has been a lot of research on air pollution and its effects on the lung function of children. But this is one of the first studies looking at the population group of young adults in a low- and middle-income country setting,’ said Otavio Ranzani, ISGlobal researcher and first author of the study.
Work involved collecting data on 1,044 people aged 20-26 years in 28 villages across the peri-urban area of Hyperbad. Lung function was measured by the researchers, with factors including sex, health behaviours, and socioeconomic background were taken into consideration, with the analysis adjusted to reflect this. Overall, household air pollution – measured in terms of biomass fuel use – was consistently found to lead to reduced lung function.
Those taking part were particularly vulnerable when unvented biomass stoves were used at home, with reductions in lung capacity rising from an average across participants of 142ml to 211ml. This is particularly worrying as such equipment is currently used by an estimated 2.6bn people worldwide. Ambient particulate matter, PM2.5, was also linked to lower lung function, although the results were less conclusive.
‘This cross-sectional study opens the doors for further longitudinal research on the effect of air pollution on lung development, especially in low- and middle-income country settings where individuals are commonly exposed to both high levels of ambient and household air pollution,’ said Cathryn Tonne, ISGlobal researcher and senior author of the study.
India currently registers more deaths from air pollution than any other country, and a recent heatwave – lasting several months – has exacerbated the situation with a dramatic increase in wildfires across many states.